Main Second Level Navigation
Jul 18, 2024
Immunoengineering the Human Heart
Bioengineering, Research
Researchers uncover role of human cardiac immune cells by engineering a model of the heart
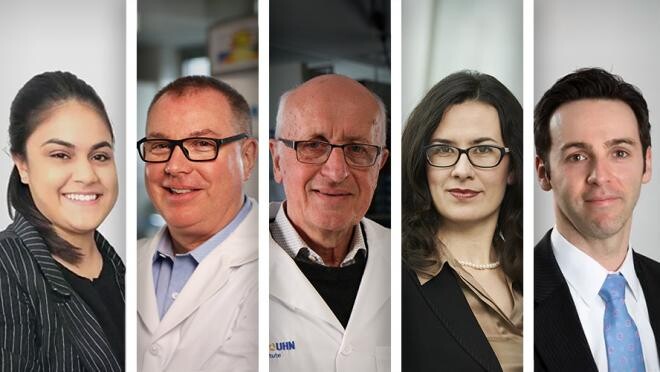
(L-R) Homaira Hamidzada, first author of the study; Drs. Michael Laflamme, Gordon Keller, Milica Radisic, and Slava Epelman, co-senior authors of the study.